The first step in understanding post-op sensitivity is to learn how the tooth feels pain.
The hydrodynamic theory of dentinal pain described by Dr. Brannstrom is the most widely accepted mechanism for how teeth feel sensitivity.

Brannstrom M. The hydrodynamic theory of dentinal pain: sensation in preparations, caries, and the dentinal crack syndrome. J Endod. 1986 Oct;12(10):453-7.The theory states that the rapid outward movement of dentinal fluid in the tubules causes sensitivity.
Before we dive into this theory, let’s review some anatomy.
Odontoblasts are large columnar cells lined between the pulp and dentin. These cells are responsible for the formation of dentin. A portion of these cells, called the odontoblast process, extend into the dentinal tubule (0.1mm). A-delta nerve fibers wrap around the process’s base and extend into the dentinal tubules. These nerve fibers receive and transmit acute pain (sharp, immediate, and short-lasting).
Another important concept to understand is capillary action, where liquid can flow in narrow spaces without external forces due to the surface tension of the enclosed area.
Let’s put this knowledge together.

When a stimulus, like air, reaches the dentin, the fluid evaporates at the opening of the tubules. Through capillary action, dentinal fluid from the pulp moves rapidly to fill in the evaporated space.
This rapid, outward movement of fluid causes deformation of the odontoblast process and A-delta nerves resulting in sharp pain. When cold reaches the dentin, it constricts the fluid in the tubules causing more space in the tubule. This sudden increase in the area creates a rapid fluid movement from the pulp into the tubule.
So we can see a common theme, to experience sensitivity, there has to be a reduction in fluid volume in the tubule. This volume change causes a rapid, outward flow of dentinal fluid that results in sensitivity.
When a smear layer is present or the tubule is blocked, stimuli such as air or sugar will not cause sensitivity as evaporation of the fluid is blocked. However, cold can still cause sensitivity as the fluid contracts, thus inducing movement.
Understanding how sensitivity happens is crucial to understanding how our bonded restorations can cause post-op sensitivity.
For this topic’s sake, we will talk about two types of bonding categories: total-etch and self-etch. The main difference is that total-etch systems need dentin etched with phosphoric acid.
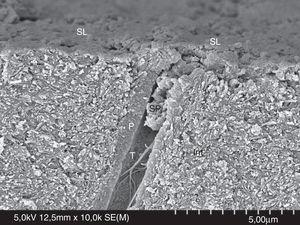
When phosphoric acid etches dentin, the smear layer and minerals are removed, resulting in the tubules being wide opened.

The etching causes a rapid, outward movement of fluid through these tubules that can cause sensitivity. These opened tubules are why a total-etch technique is more likely to cause post-op sensitivity. The adhesive’s job is to properly seal these open tubules and prevent fluid from leaking out. However, if our bonding protocol is not good, a gap can form at this level, leading to leaking fluid under our restorations and post-op sensitivity.

This OCT visual helped me understand this concept of fluid movement when there is a gap in our adhesive. Whenever a stimulus (temp or pressure) causes fluid movement in the tubules, and there is a gap in the hybrid layer, there is now an extra area the fluid can flow. As the fluid flows into the gap, the fluid volume in the tubules decreases, causing it to flow out faster. This rapid flow results in sensitivity at the nerve endings in the odontoblast process.
Conclusions: It is not normal for your patient to have ongoing post-op sensitivity after an adhesive restoration. If your patient has post-op sensitivity, it can indicate a gap somewhere in the hybrid layer. Remember that using a self-etch technique does not mean you won’t have sensitivity issues, as opened tubules can still occur in these systems. Also, not having post-op sensitivity does not mean your hybrid layer is gap-free; this just means there isn’t enough rapid outflow of fluid to cause sensitivity.
There are other reasons a patient can have post-op sensitivity. One of these reasons is cracks. Branstrom’s 1986 paper describes how he found fluid and bacteria in dentinal cracks. When a crack starts forming in dentin, fluid can leak into this area. Remember, fluid reduction followed by fluid’s rapid outward movement causes sensitivity.

The fluid moving into the crack is what causes crack tooth syndrome. Pressure applied and released during chewing causes fluid to move into these cracks that bisect the dentinal tubules. The same goes for cold, which causes the fluid to contract and rush outward into this crack.
If a crack is left behind while being restored, this can still cause sensitivity afterward since fluid can still move into the crack. That being said, not all cracks will cause sensitivity. I have seen cracks cause cusps to fracture or necrosis of the pulp, and there was never any pain.

Whenever there are deep cracks and I am unable to remove them during treatment, the patient is informed I couldn’t completely dissect the crack and there is a possibility it can lead to post-op sensitivity or necrosis.
Another factor that can cause post-op sensitivity is the rubber dam clamp causing gingival compression, leading to an exposed root surface. These sensitivities resolve with time, and I will give my patients Sensodyne to use and apply in this area before sleeping.
Occlusion is my #1 reason for post-op sensitivity. Bear with me as I tell a little story of my past failures. In my first year of practice, I had several patients who developed post-op/thermal/chewing/throbbing sensitivity after I cemented an eMax, Cerec crown.
I would make several bite adjustment appointments to the point where the articulating paper would slip through when the patient was in MIP. In the end, I would think, “it must be irreversible pulpitis!’ So I would send the patient to endo for RCT (facepalm). Except, the pain would not resolve even after RCT treatment (thermal did but not pain to biting).
Then one day, one of these patient’s informed me their crown had debonded. It took them time to get in to see me, and when they did, they informed me that the throbbing pain had subsided. It was a light-bulb moment where I realized there was some type of excursive interference I couldn’t find.
Unfortunately, I still did not understand which interference was causing the pain, and I still struggled finding it during my bite adjustments. It wasn’t until taking the mastership that I realized these patients had non-working interferences where they were hitting incline planes when the patient was chewing on the contralateral side.

These interferences were tough to find because whenever they “grind side-to-side” during adjustments, they went into working movements.
We learned the 3-paper technique during Dr. Alleman’s Mastership Program to find these interferences, and since then, I have been able to resolve all occlusion-related sensitivities.
Dr. Patrick Calalang made a great Instagram post about the 3 paper technique and how to use it to find non-working interferences. Please check it out to learn about this awesome technique.
Case Example:
This entire post was inspired by a post-op sensitivity case from my colleague Dr. Arisa Dar. She kindly let me use her case as an example of how I troubleshoot a post-op sensitivity case. This case was two premolars with DME that were cemented with eMax overlays. The teeth tested vital before treatment began. The biobased and DME were completed two weeks prior, and did not have any pain during the time between prep and cementation. The two restorations were bonded in the afternoon, and the patient started to develop pain after dinner.

My thoughts:
-Not from the rubber dam clamp since the molar has an RCT
-probably not cracks or dentin exposure since it was asymptomatic before delivery
-possible vitality issue. Need to check it again
-probably occlusion related if the pain started after eating.

Then I asked for a pre-op photo, and when I saw it, I thought the original teeth were flat, and the new overlays were made with pretty cusps. The patient was probably bumping over the new anatomy during chewing. I recommended double checking vitality, then the bite in MIP, and with the 3 paper technique.
The teeth tested vital at the follow-up visit. The patient reported she had been clenching the teeth since the cementation. The occlusion was adjusted, and the patient felt an immediate difference. The patient was also told to wear her nightguard during the day and night while the tooth settled down.
I thought everything Dr. Dar reported was a slam dunk for the sensitivity to settle down. I have found occlusion is usually the culprit when my patients feel an immediate relief in their bite after the adjustment. But the patient called the next day, saying she had pain all night again. I was stumped! But thanks to Dr. Dar’s investigative skills, she found it was the first molar causing pain.

Our thoughts are that the PA lesion was always present, and the infection flared from the excessive clenching the patient was doing after the cementation. Happy to report the patient went for retreatment of the endo, and the premolars settled down in a few days.
Post-op sensitivity can be very stressful. No one wants a patient to have pain after work they completed. I hope this post was helpful and gave you the tools necessary to think about post-op sensitivity critically.

Hi, this is a comment.
To get started with moderating, editing, and deleting comments, please visit the Comments screen in the dashboard.
Commenter avatars come from Gravatar.
I need to to thank you for this good read!! I certainly loved every bit of it. I have you bookmarked to check out new stuff you postÖ
Thank you so much!
Thank you for sharing your experience with us
Thank you for reading my post!