A Literature Review
This blog post and series will explore the concept of using liners for indirect and direct pulp caps. But first, let’s review the ideas of selective caries removal and why the biomimetic community prefers an indirect pulp cap with selective caries removal in a vital, deep caries lesion.
This paper reviews the evidence on whether complete excavation of caries is necessary and if there is evidence supporting partial caries removal.
This review found six studies regarding partial caries removal, and I will list 3 of the 6 in this post.
Mertz-Fairhurst et al. 1987:
Randomized split-mouth, four-celled design compared sealed composite restorations treated via partial caries removal with both sealed and unsealed amalgam restorations in teeth with complete excavation. The follow-up was done with radiographs at six months, one year, and two years with no significant differences among the three treatments.
Riberio et al. 1999
In one group, the clinicians removed carious dentin completely from the DEJ but only superficially from the remainder of the cavity. The second group had complete caries excavation. After X-rays and SEM analysis, they found no significant differences between the two groups.
Foley et al. 2004
They used a split-mouth design where one tooth was treated with complete caries removal and another with incomplete caries removal. The restorations were completed with copper phosphate cement with or without GIC or amalgam. The use of copper phosphate cement and GIC resulted in more abscesses. The use of GIC alone showed no significant differences between groups.
The critical review concluded: “On the basis of the studies cited in this review, one can state that there is substantial evidence that the removal of all infected dentin in deep carious lesions is not required for successful caries treatment – provided that the restoration can seal the lesion from the oral environment effectively. However, before this concept is accepted generally by the dental profession, additional clinical trials may be needed.”
In biomimetic restorative dentistry, we are taught not to use liners and only depend on our adhesive. Even if we expose the pulp, we use our adhesive system as our pulp capping material. But resin has been known to be cytotoxic to the pulp. So this next paper looks at this topic and whether adhesives can promote reparative dentin formation.

This study evaluated the pulpal response in nonexposed and exposed pulps in live monkeys. The adhesive system Clearfil Liner Bond 2 and a composite Clearfil APX was used. The samples were split into a nonexposed pulp group and a direct pulp capping group, and calcium Hydroxide was used as a control.
The teeth from the monkeys were extracted at different periods to evaluate histologically at 8, 27, or 97 days after restoration placement.
Histological data of nonexposed pulps restored with resin were:
- 43 out of 47 pulps showed no inflammation
- 4 out of 47 pulps showed either acute, chronic or severe inflammation
- 0 out of 47 were necrotic
- Of the 97 samples, 9 out of 10 showed large amounts of reparative dentin
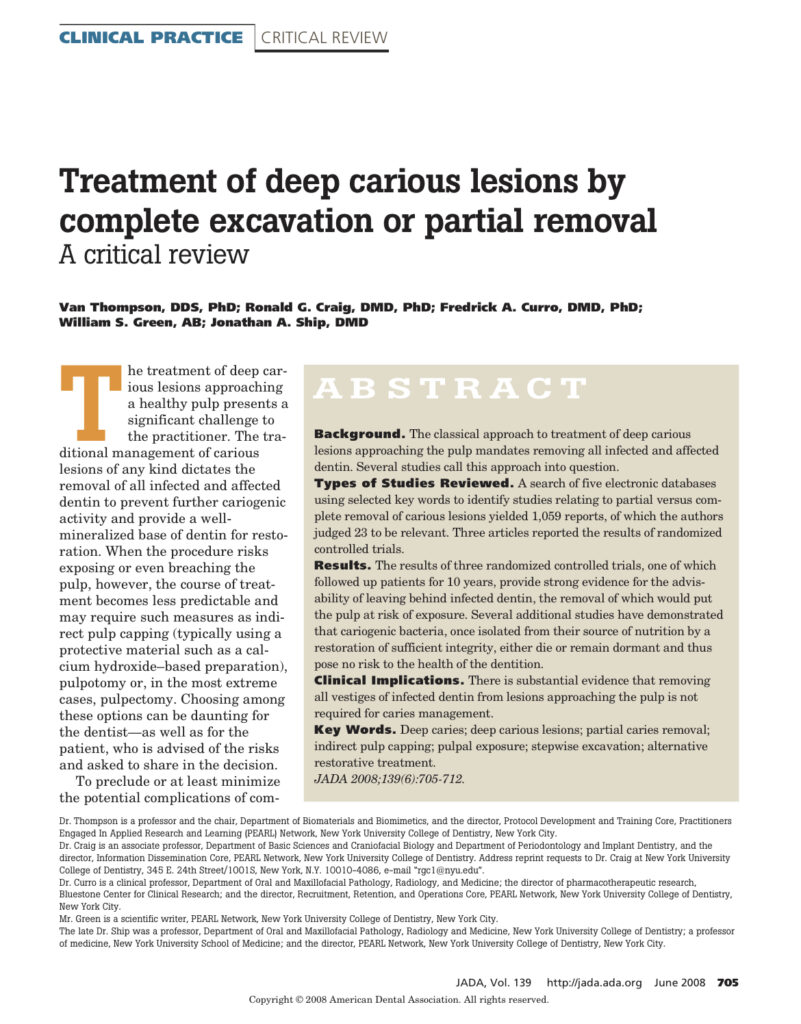
Figure A shows a sample at 27 days with the darker purple-stained dentin below the cavity on the left is the zone of the remaining dentin (150um thick). A very thin zone of reparative dentin is present.
The Ca(OH)2 controls also showed no pulpal inflammation or necrosis, with a thin layer of reparative dentin present at 22 days.
Histological data of the exposed pulps restored with resin:
- 30 out of 41 showed no inflammation
- 10 out of 41 showed either acute, chronic or severe inflammation
- 1 out of 41 was necrotic
- In the day 97 samples: 8 out of 9 samples showed new dentinal bridge formation and 7 out of 9 samples showed large bulk of new reparative dentin.
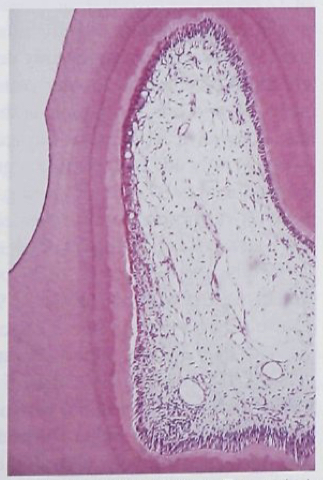
Figure B shows a 97-day sample with a dentinal bridge between the exposure (white) and the pulp. Note the tunnel defect in the middle portion of the dentinal bridge filled with cellular debris. No toxic reaction to the pulp can be seen.
Ca(OH)2 controls: 19 out of 27 samples showed no inflammation. At 35 days 14 of 15 samples showed dentinal bridging.
This study shows using an adhesive system as an indirect or direct pulp cap material has similar results to using Ca(OH)2 and does not cause toxicity to the pulp.
The authors also saw bacteria in many pulpal inflammation samples, which led them to conclude bacterial microleakage will increase the likelihood of pulpal inflammation.
The issue with Ca(OH)2 and other GI/RMGI liners is that the bond strength to sound and carious dentin is very low compared to the adhesive. So if we can prevent post-op sensitivity and promote reparative dentin with only adhesive, is there a reason for us to use liners?
Some may say Ca(OH)2 is old material with more modern options. Next time we will study these products. Stay tuned.